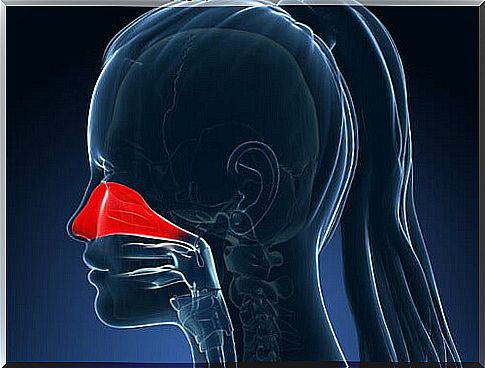
Allergic Rhinitis: Symptoms And Treatment Options

Allergic rhinitis is a chronic condition that occurs as a result of a series of reactions of the nasal mucosa due to exposure to certain external substances. This causes hyperactivity of the nose, which also affects the eyes, leading to common allergic rhinitis symptoms.
These reactions are the body’s main defense mechanism against the IgE antibodies. IgE antibodies, also called immunoglobulin E, stimulate the release of chemicals in cells predisposed to certain antigens that balance infections.
The antigens or immunoglobulins (Ig) are toxic substances that produce antibodies. Therefore, they have a defensive response to this. This chemical process puts the body in a state of immediate hypersensitivity, which manifests itself through slow inflammatory reactions.
Symptoms of Allergic Rhinitis
The symptoms can vary from person to person. However, it is not necessary for all symptoms to be present to diagnose allergic rhinitis in a patient. These are the most common symptoms that occur when it comes to allergic rhinitis:
- Daytime fatigue
- Headache
- Stuffy nose
- Nodules in the mouth-pharynx
- Changes in sleep pattern
- Itching in the nose
- Running nose
- Irregularities in the nasal mucosa
- Frequent sneezing
- Allergic reactions (bags, nose grooves)
- Symptoms of conjunctivitis (red eyes, itchy eyes, watery eyes)
- Disinterest, absent glance, half-open mouth, breathing through the mouth
- Pale nasal mucus (transparent and watery)
Related factors
There are factors associated with the development of allergic rhinitis symptoms. These include:
- Genetic predisposition
- Born in risk areas
- Early exposure to allergens
- Frequent use of antibiotics during childhood
- Family history of atopy (allergic disorders)
- Exposure to an adverse environment (tobacco, dust mites, pets)
Types of Allergic Rhinitis
There are two types of allergic rhinitis: seasonal and perennial (year-round).
Seasonal Allergic Rhinitis
Also known as hay fever, this is responsible for nearly 75% of allergic rhinitis cases. It is most common between winter and spring due to the pollination of the plants.
The characteristic symptoms of this type of allergic rhinitis include acute itching in the ears, eyes and pharynx. This may intensify with prolonged outdoor exposure, especially during pollination hours (5:00-10:00 and 19:00-22:00) and may decrease during humid and rainy days.
Perennial Allergic Rhinitis
This type of rhinitis is mainly caused by factors such as house dust mites, fungal spores (Alternia and Cladosporium) and skin particles from animals such as cats, dogs and rodents.
The allergic rhinitis symptoms may be similar to seasonal rhinitis, but the itching is less and the mucus in the nose is more watery. As a result, the patient must breathe through the mouth, talk in a nasal voice, lose the sense of smell and taste, along with other symptoms that are easier to recognize.
Common allergens
There is a large amount of allergens, but the most common are the following:
- pollen
- Enzymes
- Foods
- Medicines
- Materials (latex in gloves or probes)
- Animal secretions (hair, urine, saliva)
- Fungal spores (penicillium, cladosporium, alternaria and aspergillus)
- Mites (dermatophagoids, pteronysinus, dermatofagoides farinos, dermatofagoides microceras)
Treatment of allergic rhinitis
The treatment of allergic rhinitis usually consists of combining pharmacological and topical treatment to control allergic reactions, as well as removing allergens.
Local treatment
Topical treatment consists of a series of measures that usually need to be performed before starting any medication. This allows the patient to create an environment that promotes recovery. The measures that are part of this treatment are:
- First, avoid drastic temperature changes.
- In addition, keep the windows closed at night.
- For example, wash the nasal passages with sterile saline.
- Maintain a balanced diet and avoid foods with allergens.
- In addition, spend less time outdoors during pollination periods, windy days and peak allergen periods.
- Use an air conditioner with filter in your home and car.
- Also avoid contact with chemical irritants, from tobacco to chlorine.
- Exercise in a way that promotes constriction of blood vessels by contracting muscle fibers.
- Finally, you can use aids such as masks to reduce contact with allergens, or nasal strips to reduce nasal congestion.
Pharmacological Treatment
Today, a wide variety of medications are available to combat allergic rhinitis symptoms. These include: decongestants (anti-constipation agents), antihistamines, chromones, and nasal sprays or drops.
Decongestants for Allergic Rhinitis
These are long-acting drugs and do not cause local irritation or blockage. But they have side effects such as drowsiness, dizziness, anxiety and fluid retention. They can also raise your blood pressure.
If you use topical nasal medications (such as a nasal spray) for more than two or three days, it will decrease their effectiveness, cause a relapse, and worsen chronic rhinitis. Therefore, you should use oral decongestants instead.
Antihistamines

These are recommended for symptoms such as itching, sneezing and runny nose. However, its ability to reduce nasal congestion and eliminate allergic rhinitis symptoms is limited. Oral medications that may be more helpful for this are types such as cetirizine and loratadine.
We should mention that first-generation antihistamines can cause side effects such as drowsiness and impaired abilities. When it comes to second-generation antihistamines, there are no side effects and you feel relief almost immediately, but unfortunately it is short-lived.
Intranasal Corticoids
These drugs are effective in relieving the following symptoms: nasal congestion, runny nose, itching, and sneezing in both types of allergic rhinitis and non-allergic rhinitis.
Intranasal corticoids are absorbed quickly and also last for a long time. However, you should be careful when using them as they can have significant side effects when used for extended periods of time: stunted growth, behavioral problems, hypothalamic suppression, etc.
For example, the most recommended intranasal corticoids are:
- Flunisolide
- Mometasone Furofate
- Fluticasone
- beclomethasone
Immunotherapy
Immunotherapy consists of the gradual progressive administration of concentrations of certain extracts of allergens according to the patient’s condition. This creates a certain tolerance to the allergen.
This is the main treatment for allergic rhinitis because it is very effective. In many countries, however, the only way to apply it is subcutaneously. Therefore, patients should carefully consider factors such as the frequency of injections, duration of treatment, risks and the patient’s willingness to continue therapy.